The Story of Myelodysplastic Syndromes (MDS)
1. What is myelodysplastic syndrome (MDS)?
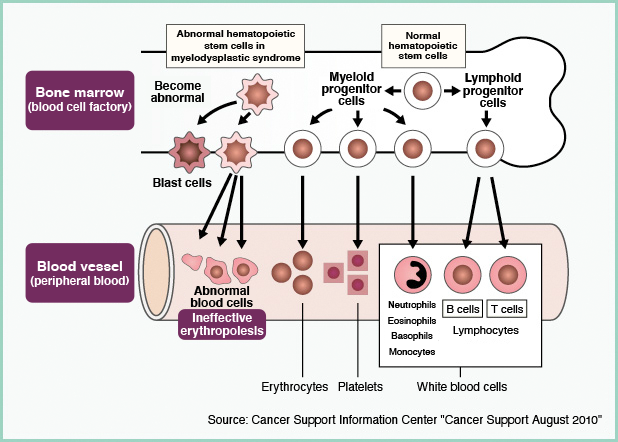
MDS is a disease in which normal blood cells (red blood cells, white blood cells, platelets) cannot be produced due to abnormalities in hematopoietic stem cells* in the bone marrow.
MDS has characteristics such as "ineffective hematopoiesis," in which immature blood cells are destroyed in the process of becoming mature blood cells, and "dysplasia," in which blood cells formed from abnormal hematopoietic stem cells have an abnormal shape. can be seen. This reduces normal blood cells and causes symptoms such as anemia, infections, and bleeding. It is also known that immature and abnormal blood cells (blasts) increase, leading to acute myeloid leukemia.
The environmental factors and genetic background that cause this disease are not well understood.
The number of MDS patients in Japan is estimated to be about 11,000. By age, the majority of MDS patients are elderly, and the male to female ratio is 2:1.
* Hematopoietic stem cells are the original cells that have both the ability to proliferate (self-replicate) and the ability to create all blood cells.
2. Symptoms of MDS
In MDS, as the number of normal blood cells decreases, symptoms may include:
Fatigue, dizziness, palpitations, and shortness of breath may occur when anemia is caused by a low red blood cell count.

Immunocompromise and weakened immunity due to a decrease in white blood cells make people more susceptible to infections and may develop a fever.

A bleeding tendency due to a decrease in platelets causes symptoms such as purpura, petechiae, and nosebleeds.
In addition, early MDS may be asymptomatic.
3. Examination of MDS
Major tests for MDS include blood tests to examine peripheral blood, bone marrow tests, bone marrow MRI tests, and chromosome tests.
- Blood test
It examines the number of red blood cells, white blood cells, and platelets in peripheral blood, the shape of blood cells, and the presence or absence of blasts. - bone marrow examination
It looks for the shape of blood cells in the bone marrow, whether there are blasts, and whether there is fibrosis in the bone marrow. - Bone marrow MRI examination
Magnetic imaging is used to check for the presence and spread of disease in the bone marrow. - Chromosome test
It looks for chromosomal abnormalities in blood cells in the bone marrow. As the disease progresses, chromosomal abnormalities increase, so it is an important test for diagnosing disease types and classifying risks.
A diagnosis of MDS is made based on the results of these tests.
4. MDS type (type)
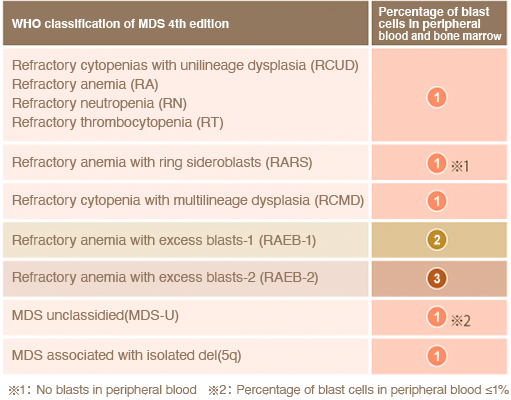
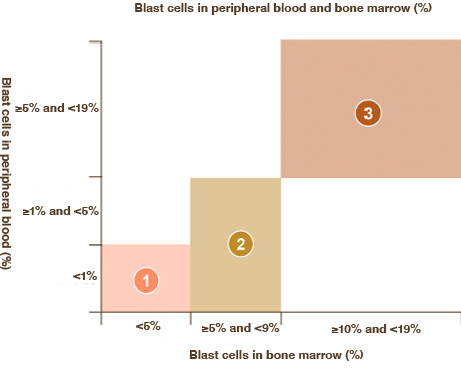
The WHO (World Health Organization) classification 4th edition was published in 2008, and classifies MDS into 7 types according to cytopenia, abnormal blood cell types, blast percentage, chromosomal abnormalities, etc. . These disease types are determined according to the test results.
What is sideroblast ring?
It refers to erythrocyte progenitor cells that have an abnormal accumulation of iron in the mitochondria, which are organelles within the cell.
What is 5q- Syndrome?
It refers to MDS with a deletion [del(5q)] in part of the long arm of the 5th chromosome. 5q- syndrome is treated as an independent subtype because of its different findings from other subtypes of MDS.
5. Risk classification of MDS
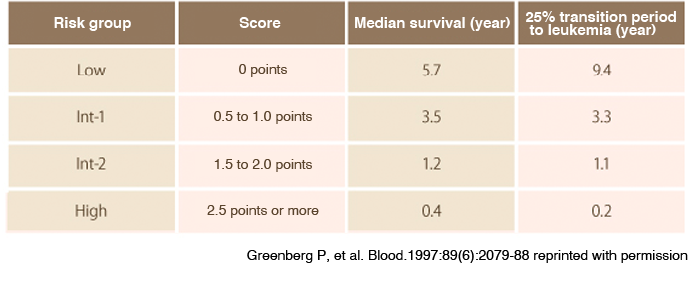
The International Prognostic Scoring System (IPSS) is widely used as a method for predicting the course of disease (prognosis). In IPSS, the percentage of blast cells in the bone marrow, chromosomal abnormalities, and cytopenia are scored, and classified into four risk groups (Low, Int-1, Int-2, High) according to the total score. Since the prognosis of MDS differs depending on the disease type, the treatment policy is determined by risk classification.
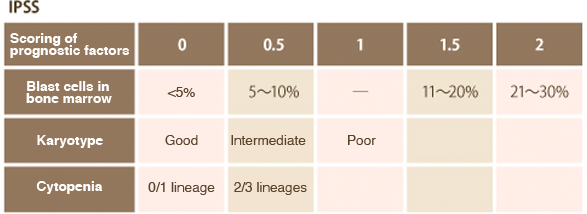
- cytopenia
Neutropenia <1,800/μL
Anemia: hemoglobin less than 10 g/dL
Thrombocytopenia <100,000/μL - Karyotype
Good: normal, chromosome 20 long arm deletion, Y chromosome deletion, chromosome 5 long arm deletion
Intermediate: Other
Bad: Complex (3 or more), Chromosome 7 abnormalities
6. Determination of treatment policy
Treatment options for MDS include supportive care, immunosuppressive therapy, chemotherapy, and hematopoietic stem cell transplantation. The patient's medical condition, general condition, and risks are assessed, and the appropriate treatment method is selected for each patient. It is also important for the patient to fully understand the treatment method for his/her own disease while consulting with the doctor, and to face the treatment together.
- supportive care
It is a treatment that compensates for the lack of blood cells by blood transfusion or drugs. Red blood cell transfusions are performed for anemia, and platelet transfusions are performed for bleeding tendencies due to decreased platelet count or decreased function. Granulocyte colony-stimulating factor (G-CSF), which has the effect of increasing white blood cells, is used for white blood cell depletion. In addition, post-transfusion iron overload adversely affects the outcome of treatment, so an iron chelator is administered. - chemical treatment
A treatment that uses anticancer drugs. It is done with the aim of reducing blasts when there are many. - hematopoietic stem cell transplantation
It is a treatment method that transplants normal hematopoietic stem cells collected from a donor (donor), and it is considered to be the only radical treatment method that can lead to cure. - immunosuppressive therapy
Immunosuppressive drugs and anti-thymocyte globulin are administered when there is a possibility that an abnormal immune response is involved in the suppression of hematopoiesis.
